A Spolight on STOMP!
As part of our commitment to helping people feel safe and lead their life, we are focused on reducing the use of, and need for, restrictive practices. In 2019 we were awarded by the UK Restraint Reduction Network as the winner for Innovative Practice in Restraint Reduction (Social Care Setting) for our restrictive practice process.
With this commitment, we pledge to reduce the over medication of people with Learning Disabilities and/or Autism (STOMP)
According to figures from Public Health England, around 30,000 to 35,000 adults with a Learning Disability are taking psychotropic medicines when they do not have the health conditions the medicines are meant for.
Individuals with Learning Disabilities and/or Autism are more likely than anyone else to be prescribed powerful psychotropic medicines which result in changes to perception, mood, or consciousness. This means that medication is being prescribed ‘off label’ as a means of managing behaviours of concern, even when alternative less restrictive and evidence-based approaches such as Positive Behaviour Support are available.
The systemic problem of over medicating people with disabilities led to the launch of the STOMP campaign in 2016 (Stopping Over-Medication of People with a Learning Disability, Autism or Both) by a consortium including, NHS England, The Royal College of Psychiatrists and The Royal College of GPs.
STOMP challenged the health and social care sectors to come together and pledge for change. TRFS met that challenge and in 2016 we pledged to:
- Promote the use of Positive Behaviour Support and provide practical ways of supporting people so they are less likely to need as much medicine, if any.
- Support individuals to have regular check-ups about their medicines
- Make sure doctors and other health professionals involve people, families, and support staff in decision making about medication.
Better Outcomes: Our Latest Progress
The Restrictive Practice Positive Behaviour Support Advisor has been supporting services across the country by working alongside staff, listening to their challenges, sharing their successes, problem solving together and supporting the implementation of our STOMP commitment.
Over the last year we have been collating organisational figures (April 2019 – March 2020) of the number of individuals we support who are prescribed psychotropic medicines by their GP for the purpose of ‘behaviour management’ (this does not include ‘as required’ medication given to treat an underlying mental health condition).
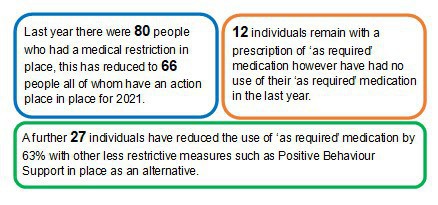
Our results show: -
A Commitment for Equality
Peter is a nonverbal man in his 30s, has a diagnosis of Autism, profound Learning Disability and Down’s Syndrome. Peter found it tremendously difficulty to attend health appointments, with waiting rooms, unfamiliar faces and a confusing understanding of expectations which led to Peter experiencing high levels of anxiety and fear that resulted in behaviours of concern.
The response from health was, ‘let’s not complete eye tests, dental checks, and chiropody appointments as this will cause too much anxiety’ was believed as the only way of managing Peter’s distress. The consequence of such an approach is Peter was left disadvantaged with ‘MOT’ appointments unchecked and an increase risk of pain and discomfort from ailments that would remain undiagnosed and untreated.
Eventually, with little exposure or experience to health services, Peter required blood tests which could not go untreated. A prescription for psychotropic medication (Lorazepam) to manage his behaviours of concern was prescribed however this was unsuccessful in helping Peter’s anxiety and led quickly to a recommendation of providing general anaesthetic for his blood tests and for any future healthcare needs that he may have.
Since we began supporting Peter, the need for blood tests have arisen again and we believed there was a better way that recognised our values to offer personalised, imaginative support that promotes the least restrictive practice to achieving outcomes. Through advocating the need to explore a range of alternative options, a collaborative relationship began that included Peter at the centre, the staff who knew him best, our Restrictive Practice Advisor and the local healthcare facilitators.
A new desensitisation programme was discussed and agreed across professions, setting out roles and responsibilities and reflecting Peter’s needs and rights to access medical care.
This new programme of care included preparatory work led by his staff team who spent time each day introducing Peter to common medical equipment used for blood tests (such as a tourniquet, syringe holder, plastic vials and dressings). Staff who knew Peter best took the lead in decision making and closely observed Peter recording when they believed he was ready to move onto the next stage in the plan.
'We agreed a time each day when we would leave equipment out for Peter to see and touch. After a couple of weeks once Peter was used to these, we started to put the tourniquet on him and show him where the syringe etc would go. Every day after being out, we would sit with Peter with his music on low and gently massage his arm where the health team had showed us the needle would most likely go in.’
Two members of the healthcare team were identified to take the bloods and be part of the process from start to finish to allow Peter to get to know the same faces and build up a familiar relationship. Through working together agreement was made for the blood test to be taking at home minimising the confusing and ever-changing environment of the surgery.
‘On the day of his test, his two nurses attended, one stroked his arm gently as we had been doing the weeks leading up to this day, a staff member also sat and held his hand and chatted to Peter to keep him feeling relaxed whilst the other nurse took his bloods. This was a complete success, all done without the need for medication, and most importantly Peter could have stopped the test at any point, it was all done under his terms, we were all so pleased and happy for Peter that he no longer had to go to hospital for this’!
Peter’s achievements mark an aspirational beginning with a new understanding of his needs and preferences paving the way for future success. Peter’s story demonstrates how the use of Positive Behaviour Support and finding individualised solutions can result in less reliance on psychotropic medication and help fulfil our pledge to reduce the over medication of people with Autism/Learning Disabilities or both.
If you would like to learn more about the work of our Positive Behaviour Support Team please email info@trfs.org.uk
Commenting is now closed on this article.